The long awaited draft on the effectiveness of homeopathy from the NHMRC has been published.
The NHMRC is Australia’s peak body for supporting research and providing health advice for Australians: doctors, governments and community members.
The draft information paper provides a scientific, objective, credible and rigorous assessment of homeopathy.
The findings were that “the quality of evidence was generally low…Based on all the evidence considered, there were no conditions for which there was reliable evidence that homeopathy was effective”.
The full draft can be found here http://consultations.nhmrc.gov.au/files/consultations/drafts/nhmrcdrafthomeopathyinformationpaper140408.pdf
A review by Edzard Ernst can be found here http://edzardernst.com
http://edzardernst.com/2014/04/the-most-thorough-and-independent-assessment-of-homeopathy-ever/
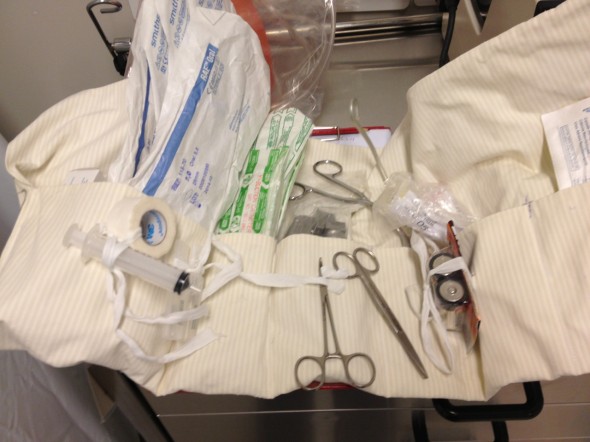
Advice on preoperative medications and homeopathic substances is in preparation and will be found under the tab “What can YOU do?”